The following survey results assess the digital readiness of organizations and their stakeholders


Step 1: Discovery
During this phase, Nurse-Family Partnership worked with Hopelab to determine what issues could be addressed with better technology and then how best to put those digital changes in place. This included examining client feedback, uncovering existing digital efforts the organization already had underway, and identifying staff who were likely to be comfortable trying new approaches. We knew staff would be more receptive to change if this phase included:
- Data showing successful digital approaches from organizations that serve the same population
- Examples within the organization where digital tools deepened rather than replaced human interactions
- Testimonials about effective innovations at other nonprofits in the same or similar fields
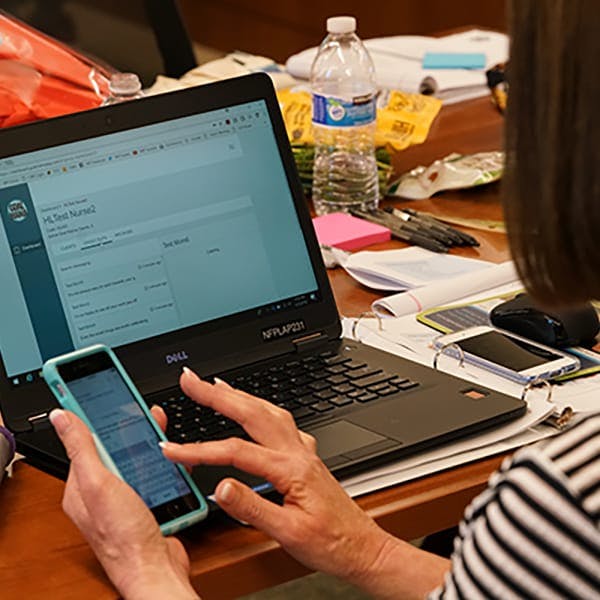
To better understand the organization’s strategy through the eyes of front-line staff, we held a three-day workshop with more than 30 nurses from Nurse-Family Partnership locations around the country. The nurses reported that moms increasingly requested resources and materials in a digital format and wanted to communicate with them between appointments through their mobile devices. We also identified key nurse and client pain points, such as clients missing appointments (“no shows”) and not having good ways to store and track goals and progress.
Following the workshop, we conducted interviews and focus groups with nurses, clients, staff, leadership, and funders. We also observed mom-nurse home visits to help determine where improvements in the process were needed and where technology could be leveraged to augment and enhance the relationship between nurse and client.
We found that sites with higher retention rates spent significant time with clients on goal setting and achievement. Moms were more likely to stick with the program when nurses worked closely with clients to identify and meet specific short and long-term goals for both themselves and their families. This led us to ask how we might build off this success by using technology to better support goal setting and track clients’ progress.
Not surprisingly, nurses worried that using an app could dilute and depersonalize the mom-nurse relationship. To address those concerns, Hopelab’s design team invited and integrated nurses’ input on how technology could be harnessed to strengthen the mom-nurse connection and not be viewed as a replacement for vital human connection.
As a general rule, this phase moves faster if nonprofits use digital surveys to gather feedback. In a study we conducted last spring of 159 nonprofit leaders, just 55 percent said they use digital surveys to solicit client feedback and many still used paper surveys.
Step 2: Developing and Testing Prototypes
Armed with an understanding of the landscape, the next step is to build and test potential digital solutions. Prototypes are tested in four key areas: how they affect outcomes; how easy they are to use; their appeal to clients and staff; and the organization’s ability to build, implement, and maintain the new technology.
Few nonprofits have the capacity to build and test digital tools. And design and technology firms that specialize in social services are in short supply. That means nonprofits may need to engage commercial firms, as was the case for Nurse-Family Partnership. The nonprofit chose Ayogo, a Vancouver, B.C.-based firm whose commercial business focuses on engaging patients in their own care, and whose staff is well versed in the principles of behavioral science.
The three partners – Nurse-Family Partnership, Hopelab, and Ayogo – worked together to create a tool that addressed the most important opportunity identified during the discovery phase: The need to help clients set and attain their goals and ways for nurses to track their clients’ progress over time.
Working with moms, nurses, and program administrators, a prototype nurse-client app called Goal Mama was developed. The app provided tools for moms to handle tasks such as setting and tracking pregnancy goals, getting resources about healthy pregnancies and parenting skills, scheduling and getting automated reminders about upcoming visits, sharing emerging needs with nurses between visits, and sharing tips with other moms.
To test the app, five nurses and 40 moms were recruited from one of Nurse-Family Partnership’s California partners — the Contra Costa Department of Public Health — to assess how the platform worked in the real world. The app was fine-tuned in response to their feedback and a larger five-site test was conducted, which included 42 nurses and 300 moms across the country. That test uncovered a key finding: Some moms found it easier to bring up sensitive topics over the app, which helped nurses better prepare themselves to address those issues at the next meeting. Additionally, the original design assumed nurses would want to use the app on their office computers, but both moms and nurses expressed a preference for a mobile app, leading to the creation of a mobile version for nurses before the product was more widely distributed.
Step 3: Distribution
A national roll-out of Goal Mama was the next step. This took a significant push from Nurse-Family Partnership’s leadership, including the creation of a new product management role for tracking and using metrics to inform ongoing changes and improvements to Goal Mama and to work with Ayogo to implement those optimizations.
The organization’s roll-out plan included in-person training of nurses across the country and the development of an online distance learning curriculum for nurses unable to attend in-person trainings. Getting the training right also took some iterative cycles of testing and refining the training, to make sure nurses were getting the support and information they needed to make the roll-out a success.
The distribution strategy also included building enthusiasm across a range of critical stakeholders. Sharing stories about the design process and insights from moms and nurses in the pilot helped create believers and champions and increased buy-in. When resistance surfaced, Nurse-Family Partnership welcomed questions and responded quickly. Feedback was also collected during this phase from users and everyone else who wanted the digital effort to succeed, resulting in product improvements such as app notifications (critically helpful during COVID-19) and better app integration with existing data collection platforms used by nurses in the field.
To date, Nurse-Family Partnership has introduced Goal Mama to 174 of its 270-plus partners and trained more than 1,500 nurses to use the app. More than 7,000 moms have begun using Goal Mama, a strong start toward the goal of expanding to 25,000 first-time moms by the end of 2021. The organization has also started several other digital initiatives, including advertising via Spotify and Pandora to attract new moms, and employing the platform Listen4Good to collect anonymous feedback on its services.
As Nurse-Family Partnership’s experience demonstrates, technology tools can help nonprofits deliver essential services more efficiently and effectively. Nonprofits of all stripes should consider upgrading their digital practices, but especially those who provide essential services such as food, shelter, and mental and emotional support.
Making these changes won’t be feasible without adequate financial support, and philanthropic funding for technology infrastructure improvements remains all too rare. Foundations need to rethink how to help grantees make this important and long overdue shift in how they provide services in the digital age. And they need to be willing to spend what it takes to get the job done.
This article originally appeared in The Chronicle of Philanthropy on November 4, 2020. The authors, Margaret Laws and Fred Dillon, thank Patricia Merino Price and Katie Smith Milway for their contributions.